Healthcare designers, industry leaders, and academics gathered in Houston for the first annual Health Forward symposium, presented by Page, to explore the innovations and inspirations driving the future of healthcare design. The questions up for discussion: How can we reach beyond the status quo to evolve and adapt? Decentralize by building bridges not walls? Embrace augmented realities and artificial intelligence (AI)? Maintain empathy and compassion? Increase access and affordability?
Hospitals Without Walls
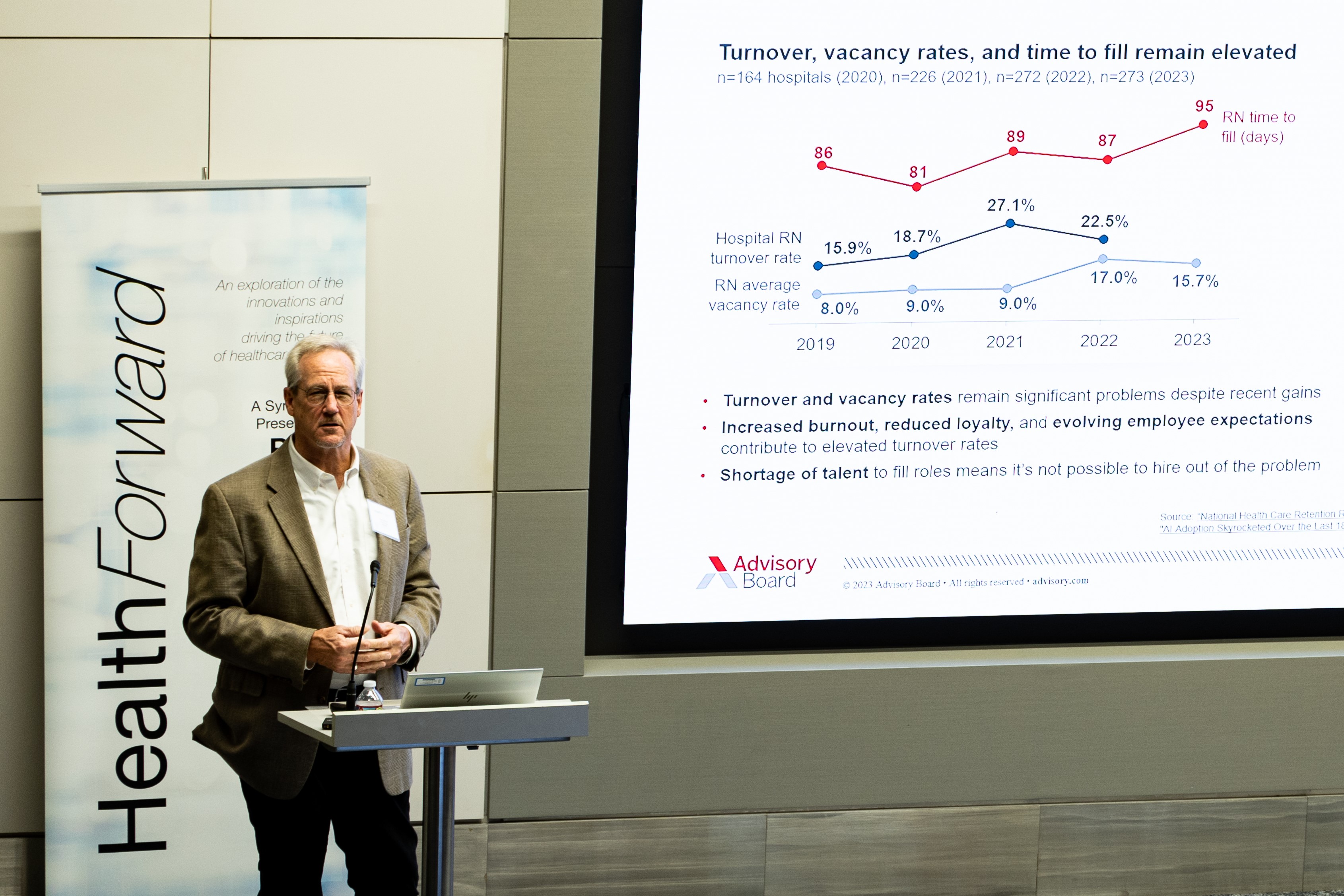 The current state of the healthcare industry is in flux, with exciting innovations on the horizon, said keynote speaker Ken Weitzel, research director and executive partner at the Advisory Board. “We just went through a three-year black swan event,” he said. The COVID-19 pandemic led to a rising need for behavioral health treatment, skipped diagnostic care and visits, undetected cancers, and a charged vaccine debate.
The current state of the healthcare industry is in flux, with exciting innovations on the horizon, said keynote speaker Ken Weitzel, research director and executive partner at the Advisory Board. “We just went through a three-year black swan event,” he said. The COVID-19 pandemic led to a rising need for behavioral health treatment, skipped diagnostic care and visits, undetected cancers, and a charged vaccine debate.
Resulting pressures are looming. Hospitals are in an “unrelenting financial struggle,” he said, with labor force costs at unsustainable levels. Recently, more than 1 million people were removed from Medicaid’s rolls. Hospitals, especially rural and community facilities, are closing, leaving residents in limbo. How is this going to impact hospital-centric service delivery? “We’re moving into a new world with complicated ecosystems,” Weitzel said. “Hospitals will not go away, but they will become one piece of the puzzle rather than the anchor: hospitals without walls.”
We’re moving into a new world with complicated ecosystems. Hospitals will not go away, but they will become one piece of the puzzle rather than the anchor: hospitals without walls.
Ken Weitzel
Increasingly, diagnostics and care can be done at home, such as tests by mail and telemedicine appointments. Large healthcare systems are bridging out from their main hospitals, with clinics and urgent care centers closer to consumers. The strategic use of advanced technology and robotics has freed nurses to work at the top of their licenses. Through medical breakthroughs, surgeries are being replaced or made unnecessary by drug therapy.
Augmented Realities
 Continuing the theme of creating new realities, speaker Stuart Corr, associate professor of bioengineering and director of innovation engineering at The Bookout Center, Houston Methodist, said we are slowly moving away from looking at screens to looking through screens – using virtual, mixed, and augmented realities to interact, converse, teach, and brainstorm.
Continuing the theme of creating new realities, speaker Stuart Corr, associate professor of bioengineering and director of innovation engineering at The Bookout Center, Houston Methodist, said we are slowly moving away from looking at screens to looking through screens – using virtual, mixed, and augmented realities to interact, converse, teach, and brainstorm.
Take, for example, the MITIE team (Houston Methodist Institute for Technology, Innovation, and Education). “When the pandemic hit, our campus was a ghost town. How did we take training and education to our customers?” Corr asked. “We created the MITIEverse – a metaverse for medical innovation with extended reality interfaces.”
When the pandemic hit, our campus was a ghost town. How did we take training and education to our customers? We created the MITIEverse – a metaverse for medical innovation with extended reality interfaces.
Stuart Corr
This takes decentralization a step further, into a world where colleagues from Mexico City and Taipei can consult with colleagues in Houston in real time, standing in a simulated auditorium or operating room, and where students can learn human anatomy through a Meta Quest headset that allows them to see a 3D orientation of a body or rotate a heart to view its chambers.
Patients over Profits
 Lawrence Hanrahan, healthcare strategic advisory director for Page, took on academic medical center myths, technology enablers, and implications for the built environment. “I had a patient remind me, ‘Young man, there’s no such thing as minor surgery,’” Hanrahan began. “Nothing is minor from the patient's perspective or when your loved ones are getting surgery. And even minor surgeries can lead to major complications.”
Lawrence Hanrahan, healthcare strategic advisory director for Page, took on academic medical center myths, technology enablers, and implications for the built environment. “I had a patient remind me, ‘Young man, there’s no such thing as minor surgery,’” Hanrahan began. “Nothing is minor from the patient's perspective or when your loved ones are getting surgery. And even minor surgeries can lead to major complications.”
Critics say academic medical centers (AMCs) are “dinosaurs whose lifetimes are limited because they can’t compete financially with smaller, private hospitals,” he said. “I don’t agree.” Hanrahan believes AMCs will continue to be the main educational facilities for all the new medical schools that need somewhere to train their students and care for the most complicated patients.
Healthcare can’t be viewed as purely a profit-driven enterprise, Hanrahan cautioned. Factors such as public health, clinical trials, and the long-term benefits of preventive care factor into the calculations. Artificial intelligence and evolving technologies seem poised to revolutionize the field. “Data is the new oil,” he said, “a raw material we will harvest and analyze for the benefit of our patients and monetize to ensure financial sustainability. Big data will drive the next paradigm shift in clinical discovery and health economics.”
Data is the new oil, a raw material we will harvest and analyze for the benefit of our patients and monetize to ensure financial sustainability. Big data will drive the next paradigm shift in clinical discovery and health economics.
Lawrence Hanrahan
Shift to Outpatient
 Joan Dentler, founder of Avanza Healthcare Strategies and an expert on outpatient strategies, weighed in on preparing for the long-term effects of outpatient migration. “The shift to outpatient services has already begun,” she said. “Patients and doctors want to be ‘in and out.’ They want services closer to home. They don’t want to go downtown and deal with traffic.”
Joan Dentler, founder of Avanza Healthcare Strategies and an expert on outpatient strategies, weighed in on preparing for the long-term effects of outpatient migration. “The shift to outpatient services has already begun,” she said. “Patients and doctors want to be ‘in and out.’ They want services closer to home. They don’t want to go downtown and deal with traffic.”
Thousands of ambulatory surgery centers (ASCs) have bloomed around the country, with many hospitals now having more than one ASC in their portfolios. More services are happening at home, from remote monitoring and wearables to telehealth follow-ups and medication adjustments. Dentler says payer pressure and patient preferences are among the top factors driving outpatient services outside hospitals.
The shift to outpatient services has already begun. Patients and doctors want to be ‘in and out.’ They want services closer to home.
Joan Dentler
What will drive outpatient services in 2040? “Refinement and proliferation of robotics, virtual reality, and 3D printing, predictive analytics for patient selection, being able to provide hospital-level care at home, and moving toward ‘right siting’ services,” she said. “This evolution will take leadership and courage, but it will emerge out of necessity.”
Decentralized Care
 Tom Redding, Sr., managing director of St. Onge, an expert on healthcare operations and analytics, emphasized that having a robotics and automation strategy is imperative to battle the never-ending labor availability challenges. “It won’t get any easier in the years to come,” he said. “As health systems continue to focus on decentralization of care, logistics will become the critical enabler for the delivery of care.” Hospitals that don’t embrace logistics as a key component to the delivery of care will be left behind, he added.
Tom Redding, Sr., managing director of St. Onge, an expert on healthcare operations and analytics, emphasized that having a robotics and automation strategy is imperative to battle the never-ending labor availability challenges. “It won’t get any easier in the years to come,” he said. “As health systems continue to focus on decentralization of care, logistics will become the critical enabler for the delivery of care.” Hospitals that don’t embrace logistics as a key component to the delivery of care will be left behind, he added.
The complexity of healthcare service delivery has also increased with the expansion of home care and telehealth, long-term care, rehab centers, surgery centers, outpatient centers, diagnostic centers, and physicians’ offices. “We can no longer independently operate each facility, replicate the same business model, manage resources and assets in a silo, or assume that labor is readily available,” he said. Disruptors include competition from non-traditional providers like CVS, Amazon, and Walmart. “Many health systems aren’t building relationships with non-traditional providers to facilitate collaborations,” he added.
It won’t get any easier in the years to come. As health systems continue to focus on decentralization of care, logistics will become the critical enabler for the delivery of care.
Tom Redding
Redding stressed that health systems must change their thinking and approach to how care is supported in many clinical settings to stay financially viable. “The current way of thinking is broken,” he said.
Questions those in the healthcare industry should be asking themselves, Redding said, are:
- How is your organization leveraging its scale and integration of services (clinical and support)?
- Does your organization have an automation and robotics strategy?
- How will home care and telehealth disrupt your organization and make your existing facilities obsolete?
- Are you investing in the right aspects of your real estate strategy?
“We can do our part to prepare our organizations for the future,” he said.
Increased Access and Innovation
 Closing keynote speaker Rubin Pillay, a medical futurist and professor of healthcare innovation at the University of Alabama, Birmingham, made some predictions and warnings about the future of health and healthcare in 2040, emphasizing that futurism is more a science than a gift bestowed on certain visionaries.
Closing keynote speaker Rubin Pillay, a medical futurist and professor of healthcare innovation at the University of Alabama, Birmingham, made some predictions and warnings about the future of health and healthcare in 2040, emphasizing that futurism is more a science than a gift bestowed on certain visionaries.
Technology is exponential not linear, becoming “cheaper, faster, better, and smarter,” he said, giving the example of laptop computers. “The end product is the democratization of a product or service, and demonetization – two major issues we face in healthcare: access and cost,” Pillay said.
“Healthcare is the only sector that, when we introduce technology in it, access goes down and prices go up,” he said, calling for healthcare business models to be adapted to align with these advances.
Technology is becoming cheaper, faster, better, and smarter. The end product is the democratization of a product or service, and demonetization – two major issues we face in healthcare: access and cost.
Rubin Pillay
We tend to overestimate the impact of a technology initially, he said, but underestimate it in the long run. Take smartphones, which were seen as fantastic communications tools at their advent but have become so much more, impacting every part of our lives. Similarly, Pillay sees AI's current hype and fears as exaggerated but said it will eventually “change the definition of what it is to be human.”
Another example of helpful technologies becoming more affordable and more widely used, Pillay said, are “all of the -omics: genomics, proteomics, microbiomics, etc. These are going to change health and healthcare radically. It took $3 billion to decode the first human genome. How much does it cost today? It's under $100 and that's in the space of two decades.”
Dozens of examples of this type of helpful convergence of technologies and medical advances exist, he said, from 3D printing with stem cells to create body parts such as corneas; brain-computer interfacing; robotic exoskeletons combined with AI; sensor technologies combined with nanoscience (such as a tattoo that measures biochemistry); organ transplants using drone delivery; and digital pain relief therapy as effective as opioids. “The power running through these innovations is in their convergence,” he said.
 And with that, the symposium segued into informal conversations, with Tushar Gupta, Page's healthcare market sector leader, reminding attendees, “Either we are part of leading change or are left behind. Health Forward allows us to explore the role of the future built environment, imagine the range of exciting possibilities, and think strategically about the actions we must take to get there.”
And with that, the symposium segued into informal conversations, with Tushar Gupta, Page's healthcare market sector leader, reminding attendees, “Either we are part of leading change or are left behind. Health Forward allows us to explore the role of the future built environment, imagine the range of exciting possibilities, and think strategically about the actions we must take to get there.”
Health Forward allows us to explore the role of the future built environment, imagine the range of exciting possibilities, and think strategically about the actions we must take to get there.
Tushar Gupta
Dive deeper into what’s possible for the future of healthcare at Health Forward.

